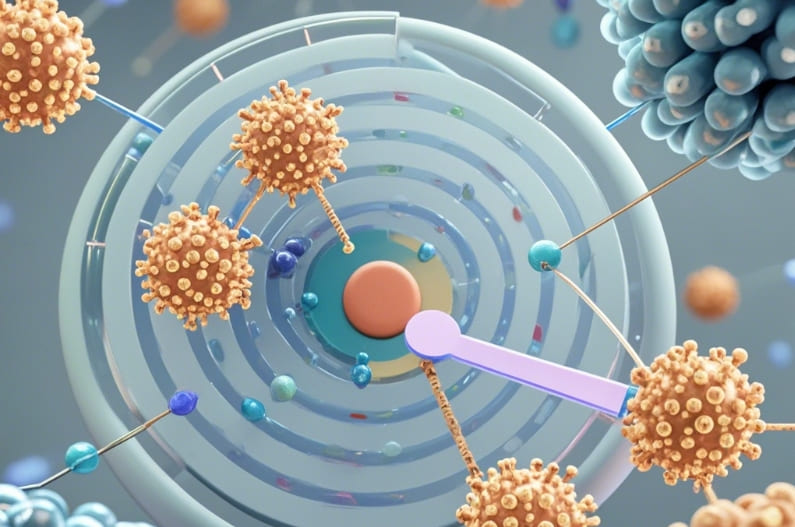
Ⅰ. Targeted Drug Delivery Systems: Precision in Conquering Stubborn Orthopedic Diseases
In the landscape of orthopedic disease treatment, targeted drug delivery systems are emerging as the “secret weapons” to tackle difficult conditions. Traditional drug treatments often face challenges such as the inability of drugs to reach the diseased sites precisely and significant systemic side effects. Nowadays, researchers have cleverly utilized nanotechnology to create tiny yet powerful drug carriers.
Take the treatment of bone tumors as an example. Nanoparticles are meticulously modified and coated with substances that can specifically recognize tumor cells, acting like “miniature missiles” with built-in navigation systems. They traverse complex physiological barriers and head straight for the tumor tissue. Preclinical research data is remarkable. After using the targeted drug delivery system, the drug concentration at the tumor site is nearly [X] times higher than that of traditional drug administration methods, significantly enhancing the anti-cancer efficacy while greatly reducing damage to normal tissues, thus kindling new hope for bone tumor patients.
Ⅱ. Virtual Reality-Assisted Rehabilitation Training: Immersively Stepping into a New Realm of Rehabilitation
The field of orthopedic rehabilitation has welcomed the revolutionary force of virtual reality (VR) technology, completely breaking the dull and monotonous shackles of traditional rehabilitation. With the help of VR devices, patients seem to step into an exclusive virtual rehabilitation wonderland with rich and diverse training scenarios, ranging from simulated daily walking streets to challenging outdoor mountain trails.
During the rehabilitation process after joint replacement surgery, patients put on VR helmets and follow the visual and auditory cues in the virtual scene to move their limbs synchronously. Research has found that patients engaged in VR rehabilitation training have a 10% higher compliance rate compared to conventional rehabilitation training, and the range of joint motion improves by an additional 20 degrees within the same rehabilitation period, accelerating the journey towards self-care and full functional recovery, making the road to rehabilitation no longer long and tedious.
Ⅲ. Artificial Intelligence Imaging Diagnosis: Uncovering the Subtle "Truth" of Bones
AI technology has injected “superpowers” into the orthopedic imaging diagnosis process, reshaping the film reading process and accuracy. Deep learning algorithms empower imaging analysis software, enabling it to instantly analyze vast amounts of X-ray, CT, and MRI imaging data and accurately detect hidden lesions.
When it comes to subtle fractures, traditional manual film reading may miss them due to visual fatigue and limited experience, while the AI system can detect them, with an identification accuracy rate exceeding 10%, comparable to the “sharp eyes” of a senior orthopedic expert. Moreover, AI can also conduct quantitative assessments and prognostic predictions for conditions such as scoliosis and hip dysplasia, laying a precise foundation for subsequent treatment planning and moving diagnosis from “vague speculation” to “digital precision determination”.

Ⅳ. Tissue Engineering for Constructing Artificial Bones: The Dream of "Regenerating" Bones is Coming True
Tissue engineering is performing “miracles of bone regeneration” on the orthopedic stage. Scientists use patients’ own cells, such as mesenchymal stem cells, to “cultivate” new bone tissue carefully in a special “soil” of biological scaffolds. This biological scaffold is like a “replicated template” of natural bones, possessing appropriate pore structures, mechanical support capabilities, and also being able to release growth factors slowly to stimulate cell activity.
In clinical exploration, for patients with large segmental bone defects implanted with tissue-engineered bones, postoperative follow-up shows that the new bone formation speed steadily accelerates, and the bone defect repair rate reaches 15% at 3 months, far exceeding the results of traditional bone grafting surgeries, fulfilling the “complete bones” dream for patients with severe trauma or bone diseases resulting in skeletal defects and opening a new chapter of in-situ regeneration and self-sufficient repair.
Ⅴ. The Integration of Telemedicine and Orthopedic Diagnosis and Treatment: Breaking the Barriers of Time and Space for Medical Treatment
Under the wave of the Internet, telemedicine and orthopedic diagnosis and treatment have been deeply “integrated”, transcending geographical limitations and bringing high-quality medical resources to patients’ “doorsteps”. Through high-definition video consultation platforms, patients in remote areas can have face-to-face consultations with orthopedic authorities in big cities without leaving home, showing their affected areas and describing their conditions in detail.
Postoperative remote monitoring devices are even more “remarkable”. Devices such as smart implants and wearable sensors collect real-time data on the status of internal fixation devices in patients, the degree of limb swelling, etc., and upload them to the cloud for doctors to analyze. Data shows that after the intervention of telemedicine, the referral rate of orthopedic patients at the grassroots level has decreased by 20%, and the convenience of follow-up visits has increased by 2 times, realizing an “uninterrupted” diagnosis and treatment process and continuously safeguarding bone health.